Narmal Vital signs: Body Temperature, Pulse, Respiratory rate (TPR) and Blood pressure
Narmal Vital signs: Body Temperature, Pulse, Respiratory rate (TPR), and Blood pressure. What are the 7 vital signs What are vital signs? Vital signs are measurements of the body’s most basic functions. The four main vital signs routinely monitored by medical professionals and health care providers include the following:
- Body temperature
- Pulse rate
- Respiration rate (rate of breathing)
- Blood Pressure
Vital signs are useful in detecting or monitoring medical problems. Vital signs can be measured in a medical setting, at home, at the site of a medical emergency, or elsewhere.
Vital signs normal range
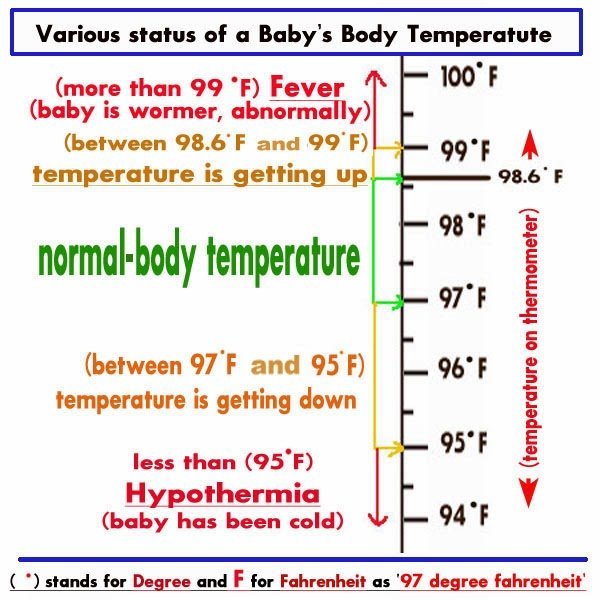
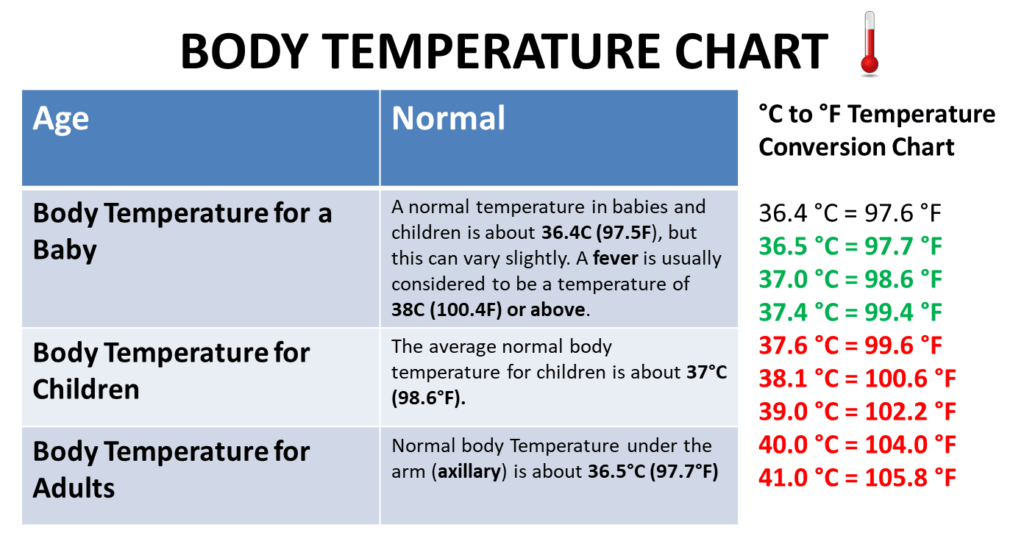
What is body temperature?
The normal body temperature of a person varies depending on gender, recent activity, food and fluid consumption, time of day, and, in women, the stage of the menstrual cycle. Body temperature can range from 97.8 degrees F (or Fahrenheit, equivalent to 36.5 degrees C, or Celsius) to 99 degrees F (37.2 degrees C) for a healthy adult.
A person’s body temperature can be taken in any of the following ways:
- Orally. Temperature can be taken by mouth using either the classic glass thermometer, or the more modern digital thermometers that use an electronic probe to measure body temperature.
- Rectally. Temperatures taken rectally (using a glass or digital thermometer) tend to be 0.5 to 0.7 degrees F higher than when taken by mouth.
- Axillary. Temperatures can be taken under the arm using a glass or digital thermometer. Temperatures taken by this route tend to be 0.3 to 0.4 degrees F lower than those temperatures taken by mouth.
- By ear. A special thermometer can quickly measure the temperature of the ear drum, which reflects the body’s core temperature (the temperature of the internal organs).
- By skin. A special thermometer can quickly measure the temperature of the skin on the forehead.
Body temperature may be abnormal due to fever (high temperature) or hypothermia (low temperature).
A fever is indicated when body temperature rises about one degree or more over the normal temperature of 98.6 degrees Fahrenheit, according to the American Academy of Family Physicians. Hypothermia is defined as a drop in body temperature below 95 degrees Fahrenheit.
About Glass Thermometers containing mercury
- According to the Environmental Protection Agency, mercury is a toxic substance that poses a threat to the health of humans, as well as to the environment. Because of the risk of breaking, glass thermometers containing mercury should be removed from use and disposed of properly in accordance with local, state, and federal laws.
- Contact your local health department, waste disposal authority, or fire department for information on how to properly dispose of mercury thermometers.
PULSE
- Definition: The pulse is a pressure wave that is transmitted through arterial tree with each heart beat following the expansion and recoil of arteries during each cardiac cycle (Marieb, Hoehn 2007).
- The rhythmical throbbing of arteries produced by the regular contractions of the heart,
- The rhythmic contraction and expansion of an artery at each beat of the heart.
Pulse Indications
- To gather information on the heart rate, pattern of beats (rhythm) and amplitude (strenght) of pulse.
- To determine the individual´s pulse on admission as a base for comparing future measurements.
- To monitor changes of pulse. (Marieb, Hoehn 2007).
Pulse Conditions where a patient´s pulse may need careful monitoring:
- Postoperative, critically ill patients
- Invasive procedure (Blood transfusion)
- Local or systemic infections, inflammations (sepsis)
- Cardiovascular conditions…
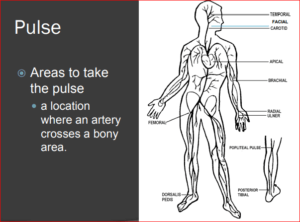
Pulse Areas to take the pulse
- A location where an artery crosses a bony area.
- http://www.medtrng.com/cls/lesson_18.htm
- FACIAL
Pulse Assessment
- Rate (frequency) per minute
- Rhythm
- Amplitude (strength, quality)
Normal vital signs for adults
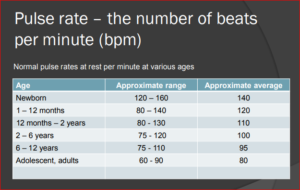
Pulse rate – the number of beats per minute (bpm)
Age |
Approximate range |
Approximate average |
| Newborn | 120 – 160 | 140 |
| 1 – 12 months | 80 – 140 | 120 |
| 12 months – 2 years | 80 – 130 | 110 |
| 2 – 6 years | 75 – 120 | 100 |
| 6 – 12 years | 75 – 110 | 95 |
| Adolescent, adults | 60 – 90 | 80 |
Pulse rate – the number of beats per minute (bpm)
- Age, Approximate range, Approximate average
- Newborn 120 – 160/ 140
- 1 – 12 months 80 – 140/ 120
- 12 months – 2 years 80 – 130/ 110
- 2 – 6 years 75 – 120/ 100
- 6 – 12 years 75 – 110/ 95
- Adolescent, adults 60 – 90/ 80
Pulse rates
- Newborns 0 – 1-month-old: 70 – 190 beats per minute
- Infants 1 – 11 months old: 80 – 160 beats per minute
- Children 1 – 2 years old: 80 – 130 beats per minute
- Children 3 – 4 years old: 80 – 120 beats per minute
- Children 5 – 6 years old: 75 – 115 beats per minute
- Children 7 – 9 years old: 70 – 110 beats per minute
- Children 10 years and older, and adults (including seniors): 60 – 100 beats per minute
- Well-trained athletes: 40 – 60 beats per minute
- Normal pulse rates at rest per minute at various ages according to the U.S.
- Department of Health and Human Services – National Institutes of Health Pulse
Pulse rate – abnormal findings
Tachycardia
- An abnormally fast heart rate; over 100 beats/min in adults (Marieb, Hoehn 2007).
- This may result from:
- Increased sympathetic response due to physical/emotional stress
- Pregnancy
- Sepsis, fever, anemia, hypoxia,
- Dehydration, hemorrhage,
- shock, hyperthyroidism,
- Cardiomyopathy, Valvular Heart Diseases, Acute Radiation Syndrome some drugs,
Bradycardia
- An abnormally slow heart rate; slower than 60 beats/min in adults (Marieb, Hoehn 2007).
- This may result from Rest, Sleep,
- A low body temperature,
- Hypothermia,
- Parasympathetic Nervous system activation
- Decreased thyroid activity,
- Hyperkalemia, an irregular cardiac rhythm, drugs (digoxin)
Pulse – rhythm
- Rhythm is the sequence of beats.
- Regular (pulsus regulars)
- Results from coordinated contractions of the heart
- Sinus rhythm
- Irregular (pulsus irregularis) – Arrhythmias
- Results from uncoordinated contractions of the heart
- Fibrilation: Rapid, irregular contractions
Pulse – strenght
- Is a reflexion of pulse strenght and the elasticity of the arterial wall
- A bounding pulse is one that is easily detected due to the exceptionally large amount of blood being pumped with each heartbeat.
- A normal, regular pulse is easy to feel and has even beats of good force.
- A weak pulse is difficult to detect due to a decreased amount of blood flowing through the arteries, usually due to bleeding or shock.
- An absent pulse cannot be detected. Lack of a detectable pulse may indicate that the artery is blocked or injured.
Pulse Amplitude abnormalities
Pulse amplitude |
Characteristics |
Conditions |
| Pulsus Magnus | A large, full pulse | Arterial hypertension |
| Pulsus parvusettardis | a weak/small pulse and very slow, late, that rises and falls gradually | Aortic stenosis |
| Pulsus alternans | alternation of large and small waves left ventricular
| dysfunction |
| Pulsus duris | A hard pulse | Atherosclerosis |
| Pulsus Mollis | A soft, easily compressible pulse hypotension | Hypotension |
| Pulsus filiformis | A thready pulse, thin as a thread, difficult to detect, usually very fast | bleeding, shock |
Radial pulse measurement
- Wash hands
- Collect equipment (wrist watch with second hand, pen, piece of paper/documentation)
- Explain procedure
- Position patient
- Place 3 fingers along the appropriate artery
- Apply light pressure on
- Count pulse 60 s.
- Record the PR on documentation
Contraindications
- Generally no
- Relative:
- Local injury, infllamation, infection,
- A-V fistula,
Assessing apical pulse rate
- Apical PR s the most reliable noninvasive way to assess cardiac function.
- Each pulsation is a combination of two sounds, S1 and S2.
- Indication – the preferred method in:
- Critically ill,
- A history of heart-related health problems,
- Cardiovascular medications.
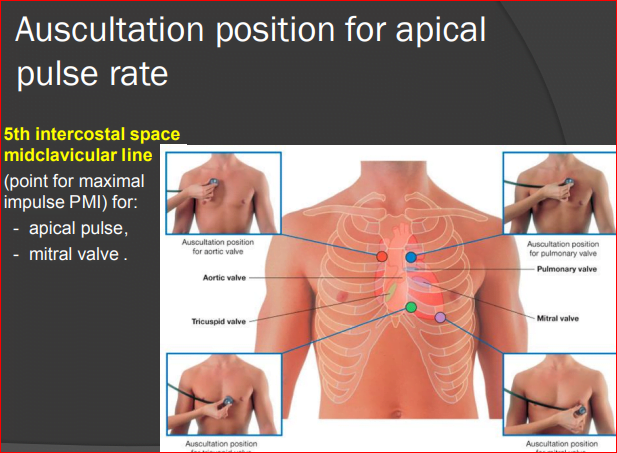
Auscultation position for apical pulse rate
- 5th intercostal space midclavicular line (point for maximal impulse PMI) for:
- Apical pulse,
- Mitral valve .
Assessing apical pulse rate
- Wash hands
- Collect equipment (stethoscope, wrist watch with second hand, pen, paper, alcohol swab)
- Explaine procedure
- Position patient
- Provide privacy
- Count the apical pulse rate while the patient is at rest.
- If the patient has been active, wait at least 5 to 10 minutes before beginning.
- Disinfect earpieces and diaphragm of stethoscope.
- Place the diaphragm of your stethoscope over the PMI and auscultate for normal S1 and S2 heart sounds. You will usually hear them as “lub-dub.” If the apical pulse is regular, count for 30 seconds, then multiply that number by 2. If the apical pulse is irregular or the patient is taking cardiovascular medications, count for 1 full minute to ensure an accurate measurement.
- Record the APR on documentation.
Basal heart rate
Normal heart rate
- The basal or resting heart rate (HRrest) is measured while the subject is:
- relaxed but awake, in a neutrally temperate environment,
- without stress, surprise.
Maximum Heart Rate
- HRmax is the highest heart rate an individual can achieve without severe problems through exercise stress and depends on age.
- Formulas:
- 220 – age
- 220 – (0.9 * age) for women
- 220 – (0.8 * age) for men
- Tanaka, Monahan, & Seals (2001) “Age-predicted maximal heart rate revisited”.
- Journal of the American College of Cardiology 37 (1): 153–6.
Optimal Heart Rate
- The best heart rate to burn body fat during exercise = optimal heart rate
- = 60% to 80% (85) of maximum heart rate.
- Age-Adjusted Method
Lower limits for training:
- HRopt = 0.60 * HRmax
- = 0.60 * (220 – age)
- = 0.60 * 220 – (0.9 * age) W
- = 0.60 * 220 – (0.8 * age) M
Upper limits
- HRopt = 0.80 * HRmax
- = 0.80 * (220 – age)
- The Karvonen Formula for HRopt.
Target Heart Rate
- = ((max HR − resting HR) × %Intensity)
- + resting HR example
Target Heart Rate
PHYSIOLOGY OF RESPIRATION
Respiration includes 2 processes:
- 1) External respiration – is the uptake of O2 and excretion of CO2 in the lungs
- 2) Internal respiration – means the O2 and CO2 exchange between the cells and capillary blood
The quality of these respiration processes depends on:
- a) Pulmonary ventilation – it means the inflow and outflow of air between the atmosphere and the lung alveoli
- b) Diffusion of oxygen and CO2 between the alveoli and the blood
- c) Perfusion – of lungs with blood
- d) Transport of O2 and CO2 in the blood
- e) Regulation of respiration
Nonrespiratory functions:
- In voice production
- Protective reflexes (apnoea, laryngospasm)
- Defensive reflexes (cough, sneeze)
- In thermoregulation
STRUCTURE OF THE RESPIRATORY TRACT
- Upper airways – nose,nasopharynx – borderline – larynx Lower airways – trachea, bronchi, bronchioles.
- The airways divide 23 times to 23 generations between the trachea and:
- Alveoli – 300 milion – total surface area 70 m2 lined pneumocytes – type I -flat cells
- Type II – producers of the surfactant
- Lymphocytes, plasma cells, alveolar macrophages, mast cells….
- Innervation: Smooth muscles innervated by
- Autonomic nervous system:
- Parasympathetic – muscarinic – bronchoconstriction – sympathetic – beta2 – receptors – bronchodilation – mainly to adrenalin
- – noncholinergic nonadrenergic innervation – VIP
MECHANICS OF VENTILATION
- Inspiration – an active process – contraction of the inspiratory muscles:
- Diaphragm – accounts for 60-75% of the tidal volume
- External intercostal muscles
- Auxiliary-accessory-inspiratory muscles: Scalene and sternocleidomastoid m.m.
- Expiration – quiet breathing – passive process – given by elasticity of the chest and lungs – forced expirium – active process – expiratory muscles: –
- Internal intercostal m.m.
- – Muscles of the anterior abdominal wall
- Innervation: Motoneurons: Diaphragm – n.n. phrenici (C3-C5)
- Others–lower segments o the spinal cord
Pulmonary ventilation
- The volume of the air inspired and expired per time unit – mostly expressed as minute ventilation MV = VT x f (6-8 l/min)
- Increase in alveolar ventilation over the requirements of the metabolism – → hyperventilation (decrease in PACO2 and increase in PAO2, the result –
- – hypocapnia – it means – hyperventilation causes respiratory alcalosis an opposite situation – hypoventilation – hypercapnia – respiratory acidosis Maximum voluntary ventilation MVV 120 – 180 l/min
Terminology
- eupnoeic – normal quiet breathing
- tachypnoea – breathing at higher frequency
- bradypnea – breathing with lower frequency
- hyperpnoea – deeper br.
- dyspnoea – laborious br.
- orthopnoea – using auxiliary muscles
- apnoea – cease of breathing
Pulmonary ventilation consists of:
- 1) alveolar ventilation
- 2) ventilation of dead space
Alveolar ventilation
- – is the amount of air reaching the alveoli
- – if the frequency of breathing is 12/min and VT is 500 ml, than minute ventilation is 6 litres.
- – If the dead space is 150 ml, than 500 – 150 = 350 ml x 12 = 4200 millilitres – alveolar ventilation is 4.2 l/min.
- Rapid, shallow respiration causes decrease of alveolar ventilation
What is High Blood Pressure?
What is High Blood Pressure? Blood pressure is the force of blood pushing against blood vessel walls. It’s measured in millimeters of mercury (mm Hg). High blood pressure (HBP) means the pressure in your arteries is higher than it should be. Another name for high blood pressure is hypertension.
Two Types of Blood Pressure (Systolic and Diastolic)
- Blood pressure is written as two numbers, such as 112/78 mm Hg.
- The top or larger, number (called systolic pressure) is the pressure when the heartbeats.
- The bottom or smaller, number (called diastolic pressure) is the pressure when the heart rests between beats.
Normal blood pressure is below 120/80 mm Hg.
- If you’re an adult and your systolic pressure is 120 to 129, and your diastolic pressure is less than 80, you have elevated blood pressure.
- High blood pressure is a systolic pressure of 130 or higher, or a diastolic pressure of 80 or higher, that stays high over time.
- High blood pressure usually has no signs or symptoms.
- That’s why it is so dangerous.
- But it can be managed.
- Nearly half of the American population over age 20, has HBP, and many don’t even know it.
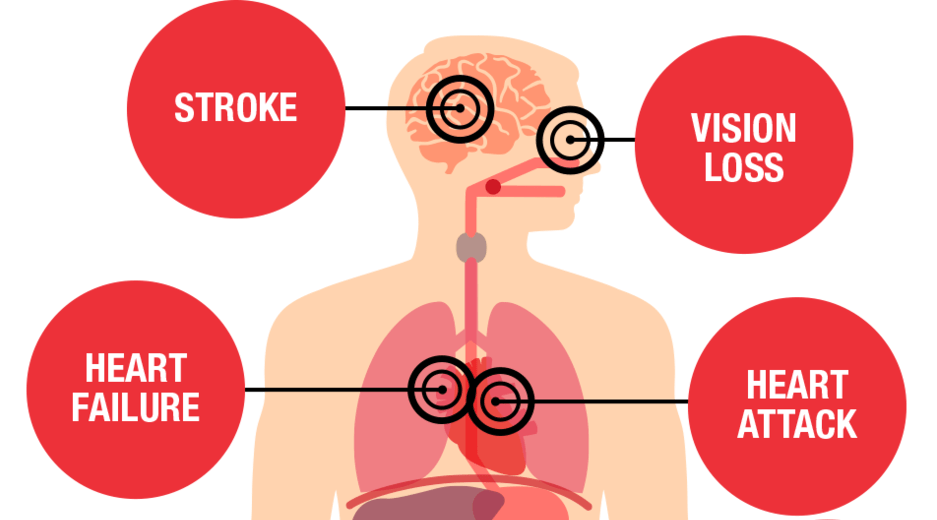
- Not treating high blood pressure is dangerous.
- High blood pressure increases the risk of heart attack and stroke.
Am I at a higher risk of developing HBP?
- There are risk factors that increase your chances of developing HBP.
- Some you can control, and some you can’t.
- Those that can be controlled are:
• Cigarette smoking and exposure to secondhand smoke
• Diabetes
• Being obese or overweight
• High cholesterol
• Unhealthy diet (high in sodium, low in potassium, and drinking too much alcohol)
• Physical inactivity - Factors that can’t be modified or are difficult to control are:
• Family history of high blood pressure
• Race/ethnicity
• Increasing age
• Gender (males)
• Chronic kidney disease
• Obstructive sleep apnea - Socioeconomic status and psychosocial stress are also risk factors for HBP.
- These can affect access to basic living needs, medication, health care professionals, and the ability to adopt lifestyle changes.
How can I tell I have it?
- The only way to know if you have high blood pressure is to get it checked regularly.
- For proper diagnosis of HBP, your health care professional will use an average based on two or more readings obtained on two or more visits.
What can I do about HBP?
- Don’t smoke and avoid secondhand smoke.
- Reach and maintain a healthy weight.
- Eat a healthy diet that is low in saturated and trans fats and rich in fruits, vegetables, whole grains, and low-fat dairy products. Aim to consume less than 1,500 mg/day of sodium (salt). Even reducing your daily intake by 1,000 mg can help.
- Eat foods rich in potassium. Aim for 3,500 – 5,000 mg of dietary potassium per day.
- Limit alcohol to no more than one drink per day if you’re a woman or two drinks a day if you’re a man.
- Be more physically active. Aim for 150 minutes of moderate-intensity physical activity or at least 75 minutes of vigorous physical activity per week, or a combination of both, spread throughout the week. Add muscle-strengthening activity at least two days per week for more health benefits.
- Take medicine the way your health care professional tells you.
- Know what your blood pressure should be and work to keep it at that level.
HOW CAN I LEARN MORE?
- Call 1-800-AHA-USA1 (1-800-242-8721), or visit heart.org to learn more about heart disease and stroke.
- Sign up for our monthly Heart Insight e-news for heart patients and their families at HeartInsight.org.
- Connect with others sharing similar journeys with heart disease and stroke by joining our Support Network at heart.org/SupportNetwork.
Do you have questions for your doctor or nurse?
Take a few minutes to write down your questions for the next time you see your health care professional.
For example Will I always have to take medicine?
What should my blood pressure be?