Hypoglycemia: Causes, Symptoms, Diagnosis and Monitoring, Treatment Options, Prevention Strategies and Risk Factors of Hypoglycemia in Diabetes
Introduction
Hypoglycemia, often referred to as low blood sugar, is a medical condition characterized by abnormally low levels of glucose in the bloodstream. The body relies on glucose as its primary energy source, and maintaining an optimal blood sugar level is crucial for overall health.
In this article, we will delve into the intricacies of hypoglycemia, exploring its causes, symptoms, effects on the body, diagnosis, treatment, and preventive measures.

Causes of Hypoglycemia
One of the primary causes of hypoglycemia is the excessive production of insulin, a hormone that regulates blood sugar levels. Skipping meals and engaging in intense physical activity without adequate fuel are also common triggers. Understanding these factors is essential for preventing hypoglycemic episodes.
Symptoms of Hypoglycemia
Recognizing the symptoms of hypoglycemia is vital for timely intervention. Shaking and trembling, sweating, and irritability are common signs. Individuals experiencing these symptoms should take immediate action to raise their blood sugar levels.
Effects on the Body
Untreated hypoglycemia can lead to severe consequences, including cognitive impairment, seizures, and loss of consciousness. It is crucial to be aware of these potential outcomes and seek prompt medical attention when needed.
Diagnosis and Monitoring
Diagnosing hypoglycemia involves blood glucose tests, which measure the concentration of sugar in the bloodstream. Continuous Glucose Monitoring (CGM) is another effective method for realtime tracking, providing valuable insights into blood sugar fluctuations.
Treatment Options
Immediate measures for addressing hypoglycemia include consuming sugarrich foods or beverages. Medications and lifestyle changes, such as regular meals and balanced nutrition, play a pivotal role in longterm management.
Prevention Strategies
Maintaining a balanced diet, consuming regular meals, and consistently monitoring blood sugar levels are key components of preventing hypoglycemia. Awareness of personal risk factors and proactive measures contribute to overall wellbeing.
Hypoglycemia in Diabetes
For individuals with diabetes, managing blood sugar levels is a constant challenge. Understanding the connection between diabetes and hypoglycemia is crucial, and implementing strategies to prevent low blood sugar episodes is essential for diabetic patients.

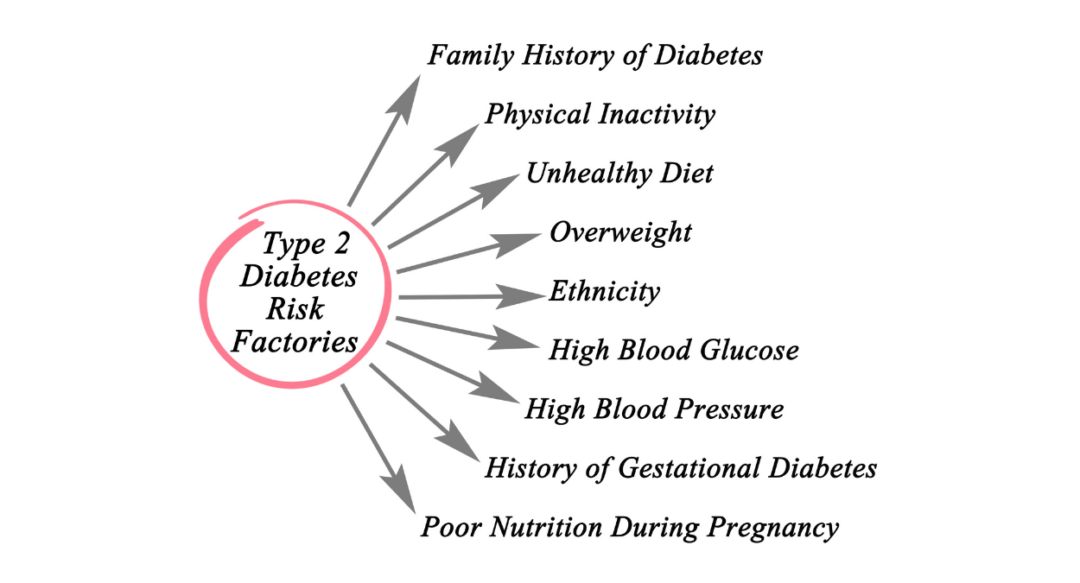
Risk Factors
Certain factors increase the risk of hypoglycemia, including type 1 diabetes, excessive alcohol consumption, and the use of specific medications. Recognizing these risk factors allows for tailored preventive measures.
Awareness and Education
Public awareness about hypoglycemia is essential, as it promotes early recognition and intervention. Educational programs targeting both the general population and individuals with diabetes contribute to a better informed society.
Emergency Response
In cases of severe hypoglycemia, administering glucagon is a critical emergency response measure. Seeking medical help promptly is imperative to prevent further complications.
Living with Hypoglycemia
Coping with hypoglycemia involves adopting various strategies and building a robust support system. Understanding one’s unique triggers and implementing personalized approaches enhances the ability to manage the condition effectively.
Research and Innovation
Ongoing research in the field of hypoglycemia continues to bring forth innovative treatment options and management strategies. Staying informed about these advancements is crucial for individuals living with or at risk of hypoglycemia.
Myths and Facts
Dispelling common myths surrounding hypoglycemia is essential for fostering a more accurate understanding of the condition. Addressing misconceptions contributes to a more supportive and informed community.
Conclusion
In conclusion, hypoglycemia is a complex condition that requires vigilant management and awareness. By understanding its causes, symptoms, and effective preventive measures, individuals can take control of their health and minimize the impact of low blood sugar episodes.
35 Frequently Asked Questions (FAQs)
1. Is hypoglycemia only a concern for people with diabetes?
No, while diabetes is a common risk factor, hypoglycemia can affect anyone, especially those on certain medications or with specific lifestyle habits.
2. Can hypoglycemia be prevented through dietary changes alone?
A balanced diet is crucial, but other factors like regular meals, monitoring blood sugar levels, and lifestyle adjustments also play a significant role in prevention.
3. What role does glucagon play in treating hypoglycemia?
Glucagon is a hormone that raises blood sugar levels and is often administered in emergency situations to counteract severe hypoglycemia.
4. How can family and friends support someone with hypoglycemia?
Offering understanding, being aware of emergency measures, and providing emotional support are essential ways to help someone managing hypoglycemia.
5. Are there any alternative therapies for managing hypoglycemia?
While lifestyle changes and medication are primary approaches, some individuals explore complementary therapies. It’s crucial to discuss any alternative treatments with a healthcare professional.
6. Is hypoglycemia only a concern for people with diabetes?
No, while diabetes is a common risk factor, hypoglycemia can affect anyone, especially those on certain medications or with specific lifestyle habits.
7. Can hypoglycemia be prevented through dietary changes alone?
A balanced diet is crucial, but other factors like regular meals, monitoring blood sugar levels, and lifestyle adjustments also play a significant role in prevention.
8. What role does glucagon play in treating hypoglycemia?
Glucagon is a hormone that raises blood sugar levels and is often administered in emergency situations to counteract severe hypoglycemia.
9. How can family and friends support someone with hypoglycemia?
Offering understanding, being aware of emergency measures, and providing emotional support are essential ways to help someone managing hypoglycemia.
10. Are there any alternative therapies for managing hypoglycemia?
While lifestyle changes and medication are primary approaches, some individuals explore complementary therapies. It’s crucial to discuss any alternative treatments with a healthcare professional.
11. What is the connection between diabetic mallets and hypoglycemia?
Diabetic mallets are not directly linked to hypoglycemia. Mallet finger injuries involve tendon damage, while hypoglycemia pertains to low blood sugar levels.
12. Can diabetic mallets affect blood sugar levels?
Diabetic mallets, being an injury, typically don’t impact blood sugar levels directly. However, stress from any health condition may indirectly influence glucose regulation.
13. Are individuals with diabetes more prone to mallet finger injuries?
Diabetes itself doesn’t increase the risk of mallet finger injuries. However, complications such as peripheral neuropathy may affect sensation and increase the risk of accidental injuries.
14. How does hypoglycemia differ from hyperglycemia in diabetes?
Hypoglycemia involves low blood sugar levels, leading to symptoms like shaking and confusion, while hyperglycemia is characterized by high blood sugar, resulting in symptoms such as excessive thirst and frequent urination.
15. Can diabetic medications contribute to hypoglycemia?
Yes, certain diabetic medications, especially insulin and some oral hypoglycemic agents, can cause low blood sugar levels if not taken as prescribed or if meals are skipped.
16. What are the warning signs of hypoglycemia in individuals with diabetes?
Warning signs include shakiness, sweating, irritability, confusion, and dizziness, among others.
17. Is it common for people with diabetes to experience mallet finger injuries?
The likelihood of mallet finger injuries in individuals with diabetes is not significantly higher than in the general population. Injury risk depends more on lifestyle and activities.
18. How can one differentiate between diabetic neuropathy symptoms and hypoglycemia symptoms?
Diabetic neuropathy symptoms involve nerve damage, leading to tingling and numbness, while hypoglycemia symptoms are more immediate and include sweating, shakiness, and confusion.
19. Can tight blood sugar control increase the risk of hypoglycemia?
Yes, maintaining tight control of blood sugar levels, while beneficial, can increase the risk of hypoglycemia. It requires careful monitoring and adjustments to medication doses.
20. Are there specific dietary recommendations to prevent hypoglycemia in diabetes?
Eating regular, balanced meals with a mix of carbohydrates, proteins, and fats helps prevent hypoglycemia. Consultation with a dietitian can provide personalized guidance.
21. Can stress contribute to hypoglycemia in individuals with diabetes?
Stress can indirectly influence blood sugar levels, potentially contributing to hypoglycemia. Stress management techniques are important for overall diabetes care.
22. Is it safe for individuals with diabetes to engage in intense physical activities?
Yes, physical activity is important for diabetes management. However, adjustments to medication and dietary intake may be necessary to prevent hypoglycemia during and after exercise.
23. Do mallet finger injuries require specific considerations for individuals with diabetes?
While the injury itself may not have specific considerations, individuals with diabetes should ensure proper wound care and infection prevention due to potential complications related to diabetes.
24. How quickly should one address hypoglycemia symptoms to avoid severe complications?
Immediate action is crucial. Consuming a source of sugar, like glucose tablets or juice, is recommended at the onset of symptoms to prevent complications.
25. Can alcohol consumption increase the risk of hypoglycemia in individuals with diabetes?
Yes, alcohol can affect blood sugar levels and increase the risk of hypoglycemia. It’s important to consume alcohol in moderation and be aware of its impact on blood sugar.
26. What role does glucagon play in managing hypoglycemia in diabetes?
Glucagon is a hormone that raises blood sugar levels. It is often used as an emergency treatment for severe hypoglycemia when the individual is unable to consume sugar.
27. Is hypoglycemia more common in certain types of diabetes?
Hypoglycemia can occur in both type 1 and type 2 diabetes. However, it is more common in individuals using insulin, especially those with type 1 diabetes.
28. Can hypoglycemia lead to longterm complications in diabetes?
Severe or recurrent hypoglycemia may have longterm cognitive effects. It emphasizes the importance of preventing and promptly treating low blood sugar episodes.
29. Are there specific strategies to prevent mallet finger injuries in individuals with diabetes?
General safety measures, such as wearing protective gear during physical activities, can help prevent mallet finger injuries in individuals with diabetes.
30. What is the role of continuous glucose monitoring (CGM) in managing hypoglycemia?
CGM provides realtime data on blood sugar levels, allowing individuals to make timely adjustments to prevent hypoglycemia. It is especially beneficial for those with fluctuating glucose levels.
31. Are there alternative treatments for hypoglycemia aside from traditional medications?
While lifestyle changes and medication are primary treatments, some individuals explore complementary therapies. These should be discussed with healthcare professionals to ensure safety.
32. Can hypoglycemia occur during sleep, and how can it be managed?
Yes, nocturnal hypoglycemia is a concern. Adjusting evening insulin doses, having a bedtime snack, and using alarms or continuous glucose monitoring can help manage this risk.
33. How does age influence the risk of hypoglycemia in individuals with diabetes?
Age can impact the risk of hypoglycemia, with older individuals potentially being more vulnerable. Medication adjustments and regular monitoring become crucial for this demographic.
34. Is hypoglycemia more common in children with diabetes than in adults?
Children with diabetes can experience hypoglycemia, but the risk may vary. Close monitoring, ageappropriate education, and communication with healthcare providers are essential.
35. Can hypoglycemia lead to psychological effects in individuals with diabetes?
Yes, the fear of hypoglycemia can cause anxiety and impact the overall psychological wellbeing of individuals with diabetes. Open communication with healthcare providers is crucial for addressing these concerns.
https://en.wikipedia.org/wiki/Diabetic_hypoglycemia#Intake_of_glucose_by_mouth

