Osteoporosis Bones Health-2023
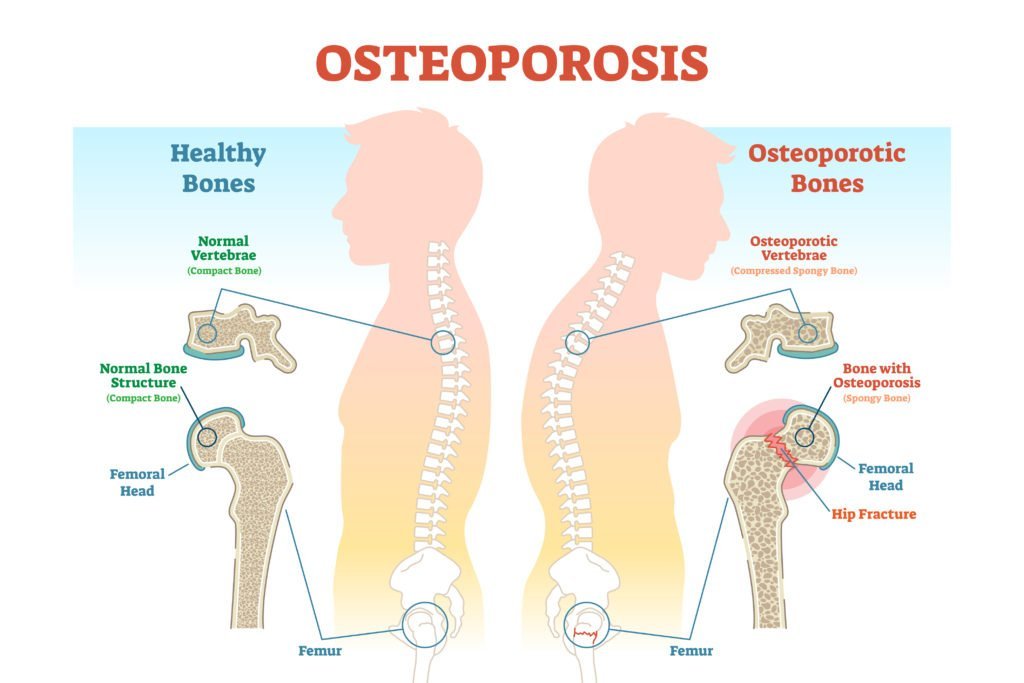
Osteoporosis Bones Health-2023. With osteoporosis, bones are brittle and often fracture or break. There are no symptoms before the osteoporosis bones shatter and the disease can only be detected through tests in your doctor’s office. You won’t automatically know your bones are getting thinner.
White and Asian women past menopause are most susceptible to the disease, but people of any age, race, or gender can get it. 8 million American women and 2 million American men have the condition. It is estimated that 50 percent of American women will experience Osteoporosis in their lifetime. If you have osteoporosis, bone health is of paramount concern.
Spinal fractures are probably the most significant concern as 20 percent of people who develop this osteoporosis bone break will die within a year. Other areas commonly affected are the hip and wrist. Hip fractures limit mobility and often result in the sufferer having to move into an assisted living facility.
Some of the risk factors for osteoporosis include being female, being under 127 pounds, having a family history of the condition, being post-menopausal, attaining an advanced age, abnormal menstrual periods, low testosterone in men, low or no dairy in the diet, having an inactive lifestyle, long term use of glucocorticoids, cigarette smoking, or drinking too much alcohol.
If you think you are at risk of osteoporosis, get a bone density scan.
The DEXA is probably the best osteoporosis bones test, but there are several others. You should have your first bone density test by the time you are 65 to establish a baseline. Thereafter, every 2 or 3 years, you should have repeat tests to monitor whether your bones are getting more brittle.
The best way to prevent getting osteoporosis is to build strong bones in the first place. As a child and young adult, having a lot of calcium in your diet can set you up for a lifetime of bone health. But it is never too late to help your bones.
One of the best things you can do for your bones is to get enough calcium in your diet or through supplements.
This is because bones are made of calcium. If you are over 50, you should get 1200 mg. of calcium a day. One cup of plain, fat-free yogurt delivers 450 mg. of calcium and one cup of milk has 300 mg. of calcium in it.
Also, you should get 400 to 600 IU of Vitamin D in your diet. Milk is also a good source of Vitamin D with 98 IU. Salmon is also an excellent source with 360 IU.
You should also become physically active when you have osteoporosis. Bones are helpful when you build muscle. Focus on a weight-bearing physical activity like walking, yoga, and lifting weights.
If you do come down with osteoporosis, several medications can help. Again, talk to your doctor about your options. If you have osteoporosis, bones’ strength becomes an important health consideration for you.
Osteoporosis Causes The Bones In The Body To Become Brittle
Osteoporosis causes the bones of the body to become brittle. In turn, they break easily. It is characterized by low bone mass and loss of bone tissue that may lead to weak bones. Those with osteoporosis, have an increased risk of fractured and broken bones, particularly in the hip, spine, and wrist.
Once thought to be a condition of old women, osteoporosis causes begin much earlier in life. Peak bone density occurs at age 25. So, it is important to build strong bones at a young age so that they will remain strong later in life. Having adequate calcium is one of the ways people build strong bones.
10 million Americans already have osteoporosis and 18 million more have a low bone mass that makes them susceptible to the disease. 4 in 5 people with osteoporosis are women. 1 in 2 women and 1 in 8 men will have an osteoporosis-related fracture in their lives.
Osteoporosis happens because an imbalance occurs between new bone formation and old bone resorption. Osteoporosis causes when the body fails to form enough new bone, too much old bone is reabsorbed, or both. Calcium and phosphate are two essential minerals for normal bone formation.
Calcium is also essential for the heart, brain, and other organs to function properly. To keep those critical organs functioning, the body may reabsorb calcium from the bones for their use. Thus, the bones may become weaker, resulting in brittle and fragile bones that can break easily.
The leading osteoporosis cause is a lack of certain hormones, especially estrogen in women and androgen in men. Women over 60 are frequently diagnosed with the disease. When women hit menopause, they have lower estrogen levels which increase their risk for osteoporosis.
Other osteoporosis causes include overuse of corticosteroids (Cushing syndrome), thyroid problems, lack of muscle use, bone cancer, certain genetic disorders, use of certain medications, and problems such as low calcium in the diet.
Risk factors include gender (women are more likely to develop osteoporosis than men), race (whites and Asians are more likely to develop the disease), post-menopausal condition, lack of regular periods, cigarette smoking, anorexia or bulimia, heavy alcohol consumption, use of corticosteroids, and use of anticonvulsants.
Early in the course of the disease, often osteoporosis causes no symptoms. Later, there may be a dull pain in the bones or muscles, particularly in the lower back or neck.
As the disease progresses, sharp pains may develop suddenly. It may be made worsened by activity that puts weight on the area. The area may also be tender. The pain generally begins to subside in one week but may linger on for more than 3 months.
Women who are past menopause and have constant pain in areas such as the neck or lower back should consult their doctor for further evaluation including risk assessment and bone density scanning.
And, that’s your rundown on osteoporosis causes.
Osteoporosis Effects On The Body
Osteoporosis affects the body by causing the bones to degenerate and lose mass. 8 million women and 2 million men in America are afflicted with the disease and at least half of all women will de osteoporosis effects in their lifetimes. There is no cure for osteoporosis, but there are treatments that will lessen osteoporosis’ effects.
Although there are currently not any cures for osteoporosis, several treatments exist that can help you to increase your bone density and prevent potential fractures. If you currently suffer from osteoporosis or are at risk for osteoporosis, you should know what the choices you have are so that you can select the correct treatment to reduce the osteoporosis effects.
Osteoporosis is when your bones lose a percentage of their mineral density.
It leads to serious fractures, including those in the wrist, hip, and spine. The fractures from osteoporosis can be painful and may even limit your independence and freedom.
The disease is most common among the elderly and women, though it can also occur in men and young people. Once you get osteoporosis, it lasts the rest of your life, but it can be reversed or reduced through careful treatment. There are numerous causes of osteoporosis including estrogen loss during menopause, eating disorders, disease, or genetic factors.
Osteoporosis is often termed the “silent epidemic” because it is accompanied by no visible symptoms.
If you suffer from osteoporosis, you probably won’t know about it until you have been diagnosed by a physician. One of the first signs is that the bones become so brittle and you suffer from a fracture or a broken bone. Fractures tend to result from everyday falls. Spinal and hip fractures are very common and the osteoporosis effects can be severe. Did you know that 20% of people with osteoporotic spine fractures die within one year?
One reason that women are more apt to develop osteoporosis is that menopause can wreak havoc on your bones. During menopause, estrogen levels in your body drop rapidly and estrogen plays an important role in bone health. The osteoclasts are kept in check by estrogen, which allows the osteoblasts to build more bone. Bones can become thin and brittle quite rapidly unless the estrogen is replaced.
Estrogen replacement is an effective treatment to lessen the osteoporosis effects. Women suffering from osteopenia or osteoporosis who take estrogen can prevent further reabsorption of bone and boost the creation of new bone mass.
Estrogen therapy is also an effective treatment for menopause.
It can increase bone mass by at least 5 percent over 2 years. It is recommended that women have at least 5 years of estrogen therapy to protect against serious fractures, including those of the hip and spine. You should know that once estrogen therapy is stopped, its benefits will begin to disappear.
Another factor to help lessen the osteoporosis effects is calcium. Calcium is essential for healthy bones. The mineral is a natural medication for osteoporosis. If you have mild to moderate osteopenia or if you have a family history of osteoporosis, calcium supplements can help reduce your risk of bone fractures. 1000 mg supplements are recommended daily, in addition to a diet rich in calcium.
And that’s the low down on osteoporosis effects.
Osteoporosis Exercises To Keep You Limber
If you are an older adult, you should begin doing osteoporosis exercises. Many people with low bone density worry that doing any exercise might lead to a fracture. But, the reality is that using your muscles can help you protect your bones. Here are some osteoporosis exercises that can help you prevent broken bones.
People who have always been physically active are less likely to have bone problems later in life. However, that doesn’t mean that people who were couch potatoes in middle age shouldn’t take up osteoporosis exercises when the condition first manifests itself.
In women, after menopause, the pace of bone loss increases. At that point, starting an exercise program is critical. It will increase your muscle strength, improve your balance and help you avoid falls — and it may keep your bones from getting weaker. Other benefits of osteoporosis exercises include increasing your ability to carry out daily tasks and activities, maintaining or improving your posture, relieving or lessening pain, and increasing your sense of well-being
There are three types of osteoporosis exercises.
The first is strength training. Strength training can include using weights, weight machines, resistance bands, or water exercises to strengthen the muscles and bones in your arms and upper spine. Strength training may work directly on your bones to slow mineral loss as well.
Osteoporosis exercises that gently stretch your upper back, strengthen the muscles between your shoulder blades, and improve your posture can all help to reduce harmful stress on your bones and maintain bone density.
The next area is weight-bearing aerobic exercises. These involve doing aerobic exercises on your feet, with your bones supporting your weight. Walking, dancing, low-impact aerobics, elliptical training machines, stair climbing, and gardening are all examples of these kinds of osteoporosis exercises.
Finally, there are flexibility exercises. When you can move your joints through their full range of motion, it helps you maintain good balance and prevent muscle injury. Additionally, flexibility helps you maintain your posture, which is essential in avoiding osteoporosis. The best osteoporosis exercises in this category are various forms of stretching. Tai Chi and Yoga are excellent forms of exercise in this category. However, you should avoid positions that may put excessive stress on the bones in your spine. These place you at greater risk of a compression fracture.
You should also avoid traditional “high school gym” kinds of exercises. These include high-impact exercises such as jumping, running, or jogging which can increase compression in your spine and lower extremities and can lead to fractures in weakened bones. Also, exercises in which you bend forward and twist your waist should be avoided. These include touching your toes, doing sit-ups, or using a rowing machine.
If you have always exercised, keep it up. If you have just been warned you have a risk of osteoporosis, now is the time to start. There are several good osteoporosis exercises to get started with.
Osteoporosis Guidelines-What Your Doctor Should Be Doing
Osteoporosis guidelines for testing are important because this is a “silent” disease. That is, you wouldn’t know you had it until you break a bone. While bone density tests allow doctors to detect it, there are no symptoms short of a broken bone or sharp pain. That’s why there are osteoporosis guidelines.
These osteoporosis guidelines are for doctors. However, if you are a patient, knowing what your doctor is supposed to do will help you know whether your physician is doing everything he or she can do to keep you from potentially deathly falls caused by osteoporosis.
Osteoporosis guidelines are for physicians who are advising patients 50 years of age or older, in particular post-menopausal women. They are supposed to advise their patients about the risk for osteoporosis and recommend a bone density test, if appropriate. In addition, they should evaluate patients for secondary causes of the disease.
Doctors following the osteoporosis guidelines will ensure that their patients are getting 1200 mg. of calcium a day and recommend supplements if that amount is not part of the patient’s daily diet. Patients should also get 800 mg. of Vitamin D per day, including supplements if necessary.
They should suggest that their patients engage in weight-bearing and muscle-strengthening exercises. This decreases the risk of fractures from falls.
Doctors are supposed to discuss the risks of cigarette smoking and excessive alcohol use vis a vis osteoporosis risk.
In addition, there are several osteoporosis guidelines related to bone density testing. All women over 65 and all men over 70 should get a baseline bone density test. Additionally, patients aged 50 to 70 who have an osteoporosis risk profile should be tested. A schedule for future testing should also be established, preferably every two years.
Osteoporosis guidelines say that doctors should begin treating patients with hip or vertebral (clinical or morphometric) fractures. After appropriate evaluation, they should also begin treatment in patients in whom dual-energy x-ray absorptiometry (DXA) shows BMD T-scores of less than –2.5 at the femoral neck, total hip, or spine.
Additionally, they should begin treatment in post-menopausal women and men 50 years and older who have a low bone mass which is also known as osteopenia. That means those with a T-score of –1 to –2.5 at the femoral neck, total hip, or spine as well as those who have a 10-year hip fracture probability of 3% or more or a 10-year all major osteoporosis-related fracture probability of 20% or more based on the US-adapted WHO absolute fracture risk model.
Currently, the Food and Drug Administration has approved bisphosphonates, calcitonin, estrogens, hormone therapy, raloxifene, and PTH 1-34 for the treatment of osteoporosis. These drugs should be discussed with patients, as appropriate.
Osteoporosis treatment is cost-effective in patients with fragility fractures or osteoporosis, in older individuals at average risk, and in younger persons with additional clinical risk factors for fracture. So, there is no excuse for a sloppy diagnosis. If you are a patient over 50 years of age, make sure that your doctor is following these osteoporosis guidelines.
Osteoporosis Medicine
The Types Of Treatments For The Condition
Osteoporosis medicine is prescribed when you come down with the disease. Osteoporosis is a disease that makes your bones brittle and susceptible to fractures and breaks. It is a serious condition. 20 percent of people who suffer from a spinal break due to osteoporosis will die within a year. That is why you want to take your osteoporosis medicine.
Post-menopausal white and Asian women are the groups most at risk for the condition. 8 million women suffer from osteoporosis and 2 million men do. It is estimated that 50 percent of women will come down with the disease at some point in their lives.
Osteoporosis has no cure but it can be treated. Osteoporosis medicine includes:
· Actinol –
Action is a bisphosphonate marketed by Aventis. Action is a prescription medication that prevents and treats postmenopausal osteoporosis. It is the only oral monthly osteoporosis treatment that has been FDA approved to help prevent fractures at both the spine and other areas where fractures commonly occur
· Boniva –
Boniva –is another bisphosphonate marketed by Roche laboratories? It comes in two forms: a tablet and an injection. There are specific guidelines for taking this once-a-month osteoporosis medication.
· Recluse –
Recluse – another bisphosphonate. It is marketed by Novartis. Reclast is the only FDA-approved, once-a-year treatment for postmenopausal osteoporosis. One annual dose, combined with daily calcium and vitamin D, will help to increase bone density, protecting and strengthening your bones.
· Didronel –
Didronel – marketed by Proctor & Gamble, Didronel tablets contain either 200 mg or 400 mg of etidronate disodium, the disodium salt of (1-hydroxyethylidene) phosphonic acid, for oral administration. This compound, also known as EHDP, regulates bone metabolism.
· Evista –
Evista – marketed by Eli Lilly, is prescribed to treat and prevent osteoporosis, the brittle bone disease that strikes some women after menopause. It is a selective estrogen receptor modulator
· Forteo –
Forteo – also marketed by Eli Lilly, is a synthetic form of parathyroid hormoneForteo is supplied in a disposable pen device that can be used for up to 28 days to give once-daily self-administered injections. Forteo is available in a 20 microgram (mcg) dose and should be taken for a period of up to 24 months.
· Fosamax –
Fosamax –is an Aminobisphosphonate marketed by Merek. It must be taken exactly as prescribed and can be lifestyle-inhibiting. However, it is a very effective osteoporosis medicine.
· Miacalcin –
Miacalcin – is marketed by Novartis. It is a synthetic form of calcitonin, a naturally occurring hormone produced by the thyroid gland. Miacalcin reduces the rate of calcium loss from bones. Since less calcium passes from the bones to the blood, Miacalcin also helps control blood calcium levels. It is a nasal spray.
Contact your doctor to see which osteoporosis treatment is right for you. When you have an illness, it is important to take your osteoporosis medicine.
https://onwebstory.com/web-stories/
https://optimalhealth.in/how-to-manage-chronic-osteoporosis-pain/